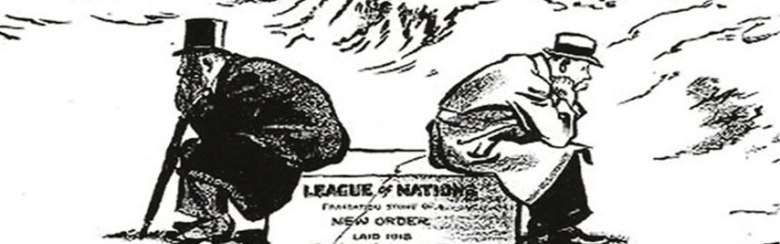
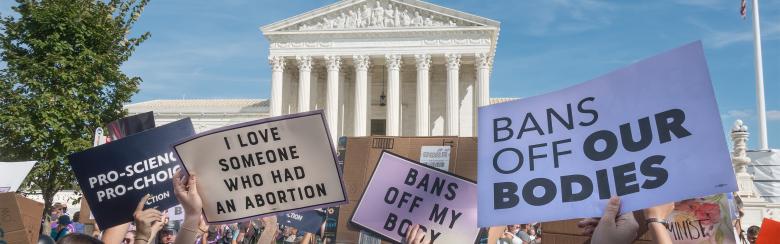
Time magazine’s 2014 ‘Person of the Year’ was Kaci Hickox, an American infectious disease public health nurse who worked in West Africa during the devasting 2014 Ebola outbreak in parts of that region. After successfully treating Ebola patients in Sierra Leone and Liberia, she returned home to a frosty welcome. Jet-lagged Hickox was put under confinement (‘quarantined’) in a medical tent at the Newark Liberty International Airport in New Jersey, though she showed no signs of illness. Three days later, she was released to return home to Maine under negotiated terms of release. A year later, she filed a suit against the state’s governor citing her confinement as a violation of her civil rights. Her grievance brought to the fore a convergence of three key questions: disease-transmission risks, the state’s power to quarantine individuals as a public safety measure and questions of individual liberty.
The overwhelmingly sudden and global eruption of the ongoing Covid-19 pandemic and its devastating toll on human lives and resources has prompted stricter public health and personal safety measures internationally. In particular, the absence of certified medications to date has partly bolstered an upsurge in preventive public healthcare strategies such as social distancing, personal hygiene measures, shutdown of public offices, stay-home orders, lockdowns, the cancellation of mass gatherings and proclamation of overseas travel bans. Governments seeking to combat cross-border influx of pandemics have adopted a decidedly more stringent set of measures such as the creation of quarantine and confinement stations at ports of entry to subject incoming travellers to preliminary tests. In so doing, apprehensions about international travels have worsened lately.
Amidst arguments about the unprecedented nature of the current outbreak, where does the coronavirus fit in the international history of pandemics?
Yale historian and author of Epidemics and Society – From the Black Death to the Present, Frank Snowden reminds us that, historically, the devastating impact of pandemics has offered states a ripe opportunity to deploy state power as a centralising authority to rally their communities, administrative personnel, civil authorities, boards of health, the military and enormous resources in a fight from which the states have often emerged stronger. Unsurprisingly, the message is that the past has something to teach the present. The work of historians in times of crises involves drawing upon the relatable past in search for precedents not to merely gratify, in the words of Marc Bloch, our “obsession with origins” but for perspectives that have timeless relevance in spite of differing contexts.
Historically, the connection between the outbreak of an epidemic and calls for an enforcement of confinement rules – often justified as legitimate public health measures for halting contagion – is conspicuous. The notion of placing a conceivably sick person in confinement is attested to by ancient texts. Some of the earliest accounts of this practice are found in the Old Testament. The books of Leviticus and Numbers, for instance, are explicit on how to quarantine lepers, based on the conceivably unclean and contagious nature of leprosy. Similarly, through a vast array of sources in the Islamic world including court registers, imperial decrees, collections of legal opinion, chronicles and plague treatises we are made to understand that Islamic scholars encouraged firm rules of quarantine for the leprous, an order that reflected a recognition of contagion.
In the fourteenth century, the world was ravaged by the bubonic plague. The Black Death, as it was known, first originated from Asia and spread to the Mediterranean. In Europe, its first point of call was Italy where it unleashed horrific devastations before crossing over to other parts of the continent. The pandemic decimated one-third of Europe’s population and ultimately spread to other continents. Italy was the hardest hit, being unfamiliar with the disease and therefore lacking any clear containment measures ahead of its influx. However, the country responded with fortitude in the face of agony. Despite lacking any advanced knowledge of microbes or theories of disease transmission, local authorities managed to trace the original vectors of the disease to sailors who had entered the area through its seaports.
Deploying substantial legal authority, Venice’s magistrates and the city’s Office of Health collaborated to devise containment measures whose primary goal was to insulate the rest of the republic against further contagion. These measures included creating the lazaretto, a makeshift dockyard of sorts where arriving vessels and cargo were isolated, cleansed and treated. Moreover, crew and passengers alike were isolated ashore and confined for forty days – a period believed to be long enough for any incipient infection to manifest fully. The forty-day period of confinement was referred to as quaranta (forty), from which we derive the term ‘quarantine.’ The term quarantine has its further origins in Ragusa, modern-day Dubrovnik, Croatia, where a law was passed in 1377 enforcing a trentino, a thirty-day isolation for visitors coming to Ragusa from infected areas. Today the word ‘quarantine’ has become a trope, bearing multiple context-specific connotations and nuances while retaining its evocative notion of confinement. However, the legacies of plague-stricken fourteen century Italy to the modern world surpass a maritime quarantine facility. Many of today’s recommended public health strategies for combating contagions and large-scale pandemics – case tracking, isolation, quarantine, the examination of travellers and imposition of barrier protection measures – are believed to be modern iterations of these earliest Venetian approaches to containment of outbreaks.
Historical parallels of what we term today as ‘epidemic’ or ‘pandemic’ exist in such vague allusions as ‘disease’, ‘plague’, ‘pestilence’ or ‘polluting disease’ in ancient literature. In classical contexts, these terms connoted either localised outbreaks or large-scale cross-border contagious diseases with massive death tolls – at least judged by the rate of diffusion and impact or scale of devastation. History’s timeline of infectious diseases is dotted with such cases as tuberculosis, leprosy, cholera, influenza, malaria, yellow fever, smallpox and syphilis.
Far from being exhaustive, what follows below is a chronological timeline of some selected ‘plagues’ that have changed world history. Rather than present them as ‘epidemics’ or ‘pandemics’, which has occasioned problems owing to the terms’ interchangeable use in scholarly literature, these are presented here under the umbrella term of infectious diseases. The selection is based on the impact of devastation as well as the public health methods deployed as containment measures, notably the use of confinement, isolation and quarantine.
430-428 Plague of Athens
Historians call it the world’s earliest documented pandemic. It ravaged the fifth century world during the Peloponnesian War, a series of conflicts between Athenians and Spartans. Believed to have naturalistic causes, the plague heavily decimated the Athenian population, contributing to its defeat at the hands of the Spartans. It then spread to Libya, Ethiopia and Egypt. While historians have debated the true diagnoses, recent research points to typhoid fever. The pandemic had distressing symptoms such as fever, vomiting, lesions and ulceration, leaving a high death toll and several fatalities. The containment strategies used included the application of purifications and incantations, and the enforcement of abstinence from baths and many food items then considered noxious to diseased people.
Plague of Justinian 541CE-755
Dubbed the “all-consuming and all-destroying plague”, it was named after Roman Emperor Justinian I under whose reign it occurred. Coinciding with the golden age of the Roman Empire – which territorially stretched from Italy to North Africa – it first originated at Pelusium in the Nile Delta in 541 CE. Subsequently, it broke out in eighteen consecutive upsurges over a stretch of two hundred years until it vanished rapidly and inexplicably in 755. The pandemic averaged five thousand deaths daily in Constantinople, depopulating cities in its wake. Its symptoms were headache, fever, leg and back pains, painful swellings, slurred speech, bloodshot eyes, hallucination, burning temperature, swollen tongue and coughing up blood. Rates of infection were high among people who lived in close confinement and in proximity to rats. The close quarters of monastic life increased the susceptibility of monks to its contagion. Sailors were similarly annihilated. The outbreak plagued Asia, Africa and Europe, leaving a ghastly death toll estimated at between twenty and fifty million in its wake. The containment strategies included unspecified traditional public health measures and quarantine.
The Japanese Smallpox Epidemic 735-737
In 735 CE, a severe epidemic of smallpox originated in the seaport province of Dazaihu on the Japanese island of Kyushu. It spread quickly and within a year had reached the island of Honshu. Its vector is believed to have been an emissary’s entourage returning from Kyushu to Honshu when he died enroute a diplomatic mission to Korean states. The returning entourage, it is believed, disseminated smallpox through the Inland Sea belt until they arrived at Honshu. By 737, the western and southern provinces of the entire island of Honshu had been infected. The death toll was one-third of the population of Japan, with some areas suffering an overwhelming mortality of sixty per cent. Victims of the disease displayed red swellings and blotches on the skin, fever, thirst and diarrhea with black or bloody stools. Japanese authorities responded to the outbreak in three ways. First, they endeavoured to provide care for the sick by distributing medicines (herbal-based remedies) among afflicted communities. Secondly, they offered free tax waivers and exemptions to entire communities, and finally sent a grain dole to afflicted provinces in response to critical emergencies. Thirdly, the state mobilised Buddhist monks in efforts to address the perceived religious causes of the disease through prayers and placatory rites. Additional medical responses to the sickness, one author informs us, included “wrapping patients in hemp or silk, keeping them warm, restraining their movements, and compelling them to eat.”
The Black Death 1347-1353
The Black death, variously referred to in fourteenth-century accounts as the “great pestilence,” the “plague of Florence,” “the mortality” and the “plague,” gained its lasting name in the eighteenth century. It originated in Central Asia in the 1330s and reached Europe in 1347 through Genoese galleys sailing from the Black Sea and docking at Messina in Sicily. It spread quickly to Sardinia, Corsica, mainland Italy and other parts of the West for six years. Its impact, however, was much longer as it lasted some five hundred years until disappearing in the 1830s. It is estimated to have decimated about half the population of Europe – a demographic disaster described by one scholar as “the worst disaster that has ever hit Europe.” Its symptoms were dark buboes and gangrene. The public health safety measures adopted included the creation of sanitary barricades manned by military detachments mandated to insulate the population by blocking movements of people and goods in and out, as well as the introduction of pesthouses, known as lazarettos (e.g., the Lazzaretto Vecchio and the Lazzaretto Nuovo constructed in the fifteen century) sited on far-flung islands where arriving ships were directed to dock for fumigation. Other measures included the introduction of the forty-day period of confinement. It was believed that the quaranta duration was enough to observe the maturation of hidden infections to certify entrants as medically safe.
Smallpox 1520
The two decades following Christopher Columbus’s arrival in the Caribbean witnessed numerous outbreaks of disease among both European and indigenous populations. Smallpox, which emerged in 1518 among the native population of Hispaniola, became the first clearly documented killer disease imported from the Old World by European visitors. The disease spread quickly, claiming one-third of the native population. From Hispaniola it spread further to other islands, reaching the Mexican mainland in 1520, coinciding with Cortés’s siege of the Aztec capital, Tenochtitlán. From central Mexico, smallpox moved into Guatemala the following year, and thereupon continued into other areas of Central America, the Andean highlands and South America where the disease is believed to have arrived sometime between 1524 and 1530 when an outbreak continued through the Inca Empire, decimating thousands of its population including several members of the Inca royal family. Brazil experienced an outbreak of smallpox in 1562, and subsequently, the disease made waves at regular intervals during the rest of the colonial period. Responses to the smallpox epidemic were varied. They include priests organising religious marches and ministering to the sick and dying. Government officials and wealthy citizens made donations for charity hospitals. In response to an exceptionally severe outbreak in 1589, the viceroy of Peru issued specific medical instructions towards helping district governments lessen the impact of the outbreak. Lima physicians advised the use of quarantine among all native communities to prevent further spread of the disease. Quarantines proved largely problematic. However, other recommended public health measures included sticking to a diet of meat, presumably to boost the immune system. One recommendation in particular was historically noteworthy: the viceroy urged families to minimise physical contact in order to prevent spreading the infection among themselves.
The 17th Century Great Plagues 1600
The city of London suffered a major epidemic of bubonic plague between April 1665 and January 1666. The total death toll is not known with certainty. Modern estimates place it at between 75,000, and 100,000. The population of the city, including its environs, was then about 460,000. In 1663, there was an outbreak of plague in the Netherlands which terrified the English government. In response the English government decreed a quarantine on movement from the Netherlands. Many Londoners left the city. The disease continued to spread at a fast pace, defeating the effectiveness of quarantine as a preventive strategy. A new set of public health policies were introduced which ordered the destruction of strayed dogs and pigs, feared as vectors of contagion. Local authorities ordered the removal of heaps of rubbish from the streets and the decongestion of ditches to ease the flow of water. Houses were fumigated and fires were lit by the streets to deter plagues. Funerary practices involving processions that attracted crowds of mourners were deemed to be modes of contagion. Attempts were made to limit attendance at such gatherings. Regulations were imposed on commerce to reduce contagious crowding. Pubs and ale-houses were closed, street vendors were prohibited to sell old clothing. Domestic travels were adversely affected as Londoners travelling to other cities claimed they were looked upon with suspicion.
Yellow Fever in Philadelphia 1793
The first main American yellow fever epidemic struck Philadelphia in July 1793 and intensified during the first weeks of October that year. Philadelphia, America’s first capital, was the most multicultural city in the nation. Its population included two thousand freed blacks as well as several white French-speaking escapees from a slave rebellion in Santo Domingo. Some key revolutionary political figures also resided there. The initial reaction of the city’s inhabitants to the epidemic was to flee. The federal authorities evacuated the city. Numerous curative measures were deployed to no avail. The cause of the disease was unknown, leading to several speculations about its origin. Opinions were divided between those who thought that the disease was locally caused by insanitary conditions and those who argued that it was imported. As J. H. Powell, author of the first major study on the issue tells us, “most medical opinion favoured importation, contagion and quarantine.” Suspicion grew that the Santo Domingan, a recently-captured vessel had brought the disease in. Following the Venetian model, a lazaretto was constructed to halt ships, inspect crew and cargo and quarantine sailors. Quarantine failed, however, as the disease was eventually found to be carried by mosquitoes. In all, out of its total population of forty-five thousand, Philadelphia was decimated by as many as five thousand. A further seventeen thousand fled.
The Cholera Outbreak 1817-1961
The delta of the Ganges and Brahmaputra Rivers is known to be the endemic home of cholera, though scholars are in dispute over the exact date of its inception. By the early 19th century cholera was unknown outside India until it erupted into a major epidemic in 1817. Soon afterwards, it spread beyond India reaching Europe in 1830 and exerting a devastating transnational sweep, resulting in seven sequential pandemics: (i) 1817–1823: Asia, (ii) 1830s: Asia, Europe, North America, (iii) 1846–1862: Asia, Europe, North America, (iv) 1865–1875: Asia, Europe, North America, (v) 1881–1896: Asia, Europe, (vi) 1899–1923: Asia, Europe, and (vii) 1961–the present: Asia, South America, Africa. Part of the reason it had remained contained in India until the start of the nineteenth century was because of the delicate nature of its causal bacterium – Vibrio cholerae – a bacterium that could not travel easily. In subsequent years, a range of factors immensely increased the rate of human travels between India and the West, three of which were key: British colonialism (bolstered by the movement of troops and trade); fairs and religious pilgrimages (the Hajj) which brought Indian Muslims to Mecca; and the revolutions in transport (railroads, steamships and the Suez Canal). These advances facilitated the bacterium’s entry to the West. Upon arrival, its oral-fecal mode of transmission found favourable conditions to thrive. These conditions were precisely the pathologies created by the Industrial Revolution – disordered urbanisation, rapid demographic growth, congested slums with scanty and unwholesome water supplies, shoddy housing, poor diet, pervasive filth and a dearth of cesspits. The port cities of Hamburg, Marseille, Naples and Valencia provided ideal conditions for its spread. Its symptoms included violent discharge of fluid from the digestive tract, sudden illness and in extreme cases, instant death. Its effects included high case fatality rates and a penchant for infecting the aged. Responses to its onslaught included mass flights, riots, social hysteria, scapegoating and economic disruption. Cholera’s devastation evoked comparisons to the fourteenth century plagues and spawned several eerie nicknames such as “the gypsy,” “the monster,” “blue cholera” and “king cholera.” Most European cities initially found cholera’s mode of transmission a mystery, questioning whether it was contagious. In search for an answer, they tried many experimental theories of disease transmission and control with mostly failed outcomes. Yet there were also the contagionists – people who preferred to call cholera a contagion before actual proof came out. Preferring to err on the side of caution, such persons strongly advocated for quarantine as a safety measure. England, France, Russia, Austria-Hungary and Prussia were home to many contagionists who drew caution from historical experiences with the plague to prescribe the imposition of quarantine and restrictions on travel. As Christian McMillen tells us, “states revived the practice of imposing a cordon sanitaire (sanitary border) in an attempt to keep cholera out; they kept careful tabs on the sick and the suspected sick, isolating them when possible; they blocked off infected zones; and they zealously disinfected, cleansed and fumigated goods and people.” In the 1830s, Russia enforced restrictions on movements yet “popular displeasure at the severe restrictions placed upon daily life, and the merchant class’ vehement opposition to quarantine and its effects on trade caused a shift to take place.”
The Third Plague 1855
This pandemic originated from Central Asia, exploding in China in 1855. It invaded Canton and then Hong Kong in 1894 and later spread on to major cities and epicentres of international commerce such as Buenos Aires, Honolulu, Sydney, Cape Town, Naples, Oporto and San Francisco. From these cities, it made sweeping incursions into some of the world’s most impoverished countries. Eighty thousand people fled Hong Kong out of panic. The pandemic devastated India, killing between thirteen to fifteen million deaths between 1898 and 1910. In West Africa, Senegal was hit hard by it in 1914, disrupting the country for the next thirty years. In the Portuguese city of Oporto, maritime quarantine was introduced which had the effect of halting the city’s commercial activity. The containment measures that were efficiently put in place included surveillance systems, maritime quarantines and isolation of victims. Christian McMillen shows that in some places city officials deployed brutality and heavy-handedness to enforce compliance with strict public health measures. In the Egyptian city of Alexandria, “health officials enlisted local leaders to gain the trust and cooperation of the citizenry. As a result, mass panic was avoided, and Alexandria’s epidemic burned out in a few months.”
The Russian Flu 1889-1890
In December of 1889, this outbreak entered Europe from the east and thus earned its nickname, the “Russian flu.” Transatlantic shipping efficiently bolstered its spread over western Europe and from there it landed in North America in the same month. It then hit Nebraska, Saskatchewan, Rio de Janeiro, Buenos Aires, Montevideo, and Singapore. By March 1890, it had entered New Zealand and soon becoming widespread in Asia and Africa, continuing to extend further into other regions of the world. An estimate of 250,000 died in Europe, though the total number of deaths globally is estimated to have been two or three times more. A bulk of this pandemic’s casualties were the aged and elderly.
The Spanish Flu pandemic 1918-1919
Between August 1918 and March 1919, while the First World War was ongoing, the world experienced a catastrophic outbreak of a highly contagious respiratory disease called the Spanish influenza. This pandemic had such a sweeping global reach that one recent scholar has cautioned that “to isolate it geographically for study is to understate its presence and impact.” Though the pandemic did not originate in Spain, it was named after it because Spain, neutral in the ongoing war, lent uncensored media reportage to its own morbidity. The flu was first detected in March 1918 in US troops training at Camp Funston, Kansas. It soon spread to every continent partly through war-time military mobilisation, infecting one-third of the world’s population and claiming over fifty million lives. Its death toll outnumbered those who perished in the war. There were no effective drugs or vaccines at that time to combat it. Most of its infected victims experienced aches and fever which worsened over days, sometimes abruptly. In Chicago, for instance, a group of school children went to class looking healthy but by lunchtime were found lying prostrate. Shoppers collapsed and died on the streets before they could be taken to the hospital. There was widespread fear and panic. As a public health strategy, patients were urged to stay home for several extra days upon the detection of relapses among those who resumed their normal routines too quickly. At a critical stage of its spread, the infection prompted precautionary measures that bear striking resemblance to the current efforts at fighting COVID-19: authorities or owners closed gathering places – theatres, cinemas, schools, places of entertainment and public transport systems. Masks were distributed. Although the disease continued to spread to various parts of the planet, keeping people apart reduced the level of infection – if such isolation could be sustained. In Atlanta, many local authorities did not sustain it; more commonly, people found that they had to go to work, and public transportation was their only means of doing so. Employers were not necessarily sympathetic to weeks – even unpaid weeks – off the job.
The Asian Flu 1957-1958
The Asian Flu was first identified in China in late February 1957 and by June 1957 it had spread to the United States. It caused in seventy thousand deaths in the United States and two million globally.
HIV Aids 1981-present
In 1981, the United States’ Centers for Disease Control reported of the outbreak of strange infections and signs of pneumonia and cancer among some male patients in New York and California. It was discovered that in all the cases, the immune systems of the patients had mysteriously collapsed. By the end of 1981, a further 189 of such cases were recorded with further escalations occurring in the next three years. A concentration of cases of failed immune systems was discovered among sexually-active male homosexuals. For a time, this syndrome was called Gay-Related Immune Deficiency (GRID). The practices of homosexuals as well as the substances they used became the focus of GRID-related medical research. Sometime later, medical researchers further discovered that there were other populations outside the gay category who also suffered from this condition, rendering the term GRID inaccurate. In the course of 1982, a new name – Acquired Immune Deficiency Syndrome (AIDS) – came into use. In 1983, two different scientific research teams, one from the Pasteur Institute in Paris, the other from the National Institutes of Health in Maryland independently detected examples of a peculiar type of viruses called retroviruses as the disease’s probable vector. The two teams reached a consensus that the ravages caused to human immune systems was caused by a retrovirus. In 1986, the name human immunodeficiency virus (HIV) became internationally certified as the name of the virus that caused the AIDS. HIV AIDS is transmitted through sexual contact, transfusion of contaminated blood, and mother-to-child transmission. Victims may develop flu-like symptoms – high fever, muscle pain, headaches and diarrhea – followed by a weakening of the immune system and additional symptoms such as weight loss, fever, skin infections and cough. There is no known cure for HIV AIDS to date. However, advances in medical research have produced antiretroviral drugs which enable patients to maintain a functional immune system. To date Sub-Saharan Africa remains the worst hit in cases of HIV AIDS infections.
SARS 2002-2003
Dubbed as the “the first pandemic of the twenty-first century,” Severe Acute Respiratory Syndrome (SARS) first appeared in the Chinese region of Guangdong in November 2002. It exploded rapidly to become an international health menace in March 2003. WHO became aware of it and declared an international travel alert. SARS was a respiratory disease characterised by dry coughs, fever, headaches and body pains, and was transmitted through droplets discharged from sneezes and coughs. It infected 8,098 people, caused 774 deaths and precipitated travel bans in several countries and even ignited the cessation of international travels into certain regions According to Frank Snowden, it caused $60 billion in “gross expenditure and business losses to Asian countries alone.” From China, SARS spread mainly by airplane to cities such as Singapore, Hong Kong and Toronto. In all, it affected twenty-nine countries and five continents, exhibiting notoriety for being “no respecter of prosperity, education, technology or access to health care” – an attribute that foreshadowed many of the currently trending features of Covid-19. By early July 2003, WHO had announced an end to its spread. Containment policies followed traditional methods akin to seventeenth century public health strategies for curbing bubonic plagues: case tracking, isolation, quarantine, the dissolution of mass gatherings, the examination of travellers, recommendations for improved personal hygiene and barrier protection by means of masks, gloves, gowns and eye protection. Although SARS affected twenty-nine countries and five continents, the containment operation successfully limited the outbreak.
The Swine Flu 2009-2010
In 2009, the world’s media was alerted to an outbreak of influenza, the ‘Swine Flu’ (H1N1), which had purportedly spread from pigs to humans in Mexico. Its origins were quickly traced to the town of La Gloria, which had witnessed cases of a severe respiratory illness since March 2009. By mid-March, about sixty per cent of the village’s inhabitants were reportedly ill with flu-like symptoms. Popular perceptions attributed the disease to infection from a nearby pig-rearing farm owned by the giant corporation Smithfield Foods. Smithfield and the Mexican government later denied this. This substantially affected the politics of global responses to it. By April 2009, 1,800 cases of swine flu had been recorded in Mexico along with several deaths. The numbers of suspected cases rose to 1,995 and by the end of the month 149 victims had died. Tourists and business folks returning from Mexico facilitated the spread of the disease abroad. By late April, the US had confirmed forty cases, Canada six, United Kingdom two, Spain one, in addition to suspected cases in other countries. The virus was detected to be easily transmitted between humans, signaling its devastating potential. Many countries and governmental organisations issued prompt calls for emergency measures to prevent travel to and from infected regions. The WHO, the European Union, diplomats, business circles, scientific experts, health officials and medical experts found themselves caught up in a maelstrom of cautionary and counter-cautionary altercations over modes of containment, all in the interest of safeguarding intercontinental travels. The WHO declared it a pandemic on the 11 June 2009 which further heightened media interest and worries globally. In many countries, numerous private and the public sector employees were alerted to safety and preventive steps. Schools and public places which experienced outbreaks were closed. China quickly deployed measures it had previously used in controlling SARS, and these included the implementation of rigorous quarantine against all persons suspected of being infected. Further, they introduced screening at airports to detect arriving foreign nationals with high temperatures, and placed them in quarantine. Chinese nationals returning from countries severely affected were placed in quarantine for ten days irrespective of their physical condition. Some Western countries also resorted to measures of biosecurity leading to a resuscitation of protectionist predispositions. In April 2009, several countries announced embargos on imports of pork produced in Mexico and the United States.
MERS 2012
In 2012, a viral respiratory infection called Middle East Respiratory Syndrome Coronavirus (MERS-CoV) was first detected in a patient at a hospital in Jeddah in Saudi Arabia. The disease upsets the respiratory tract resulting in fever, cough, breathing difficulties and fatalities. Bats were believed to be the virus’ natural reservoir, although the dromedary was considered to be the transitional host responsible for direct transmission to humans. Since 2012, there has been at least 2494 laboratory-confirmed cases of MERS-CoV related infections with at least 858 deaths according to the World Health Organization’s updates. Several countries in Middle East – Saudi Arabia, United Arab Emirates, Qatar, Jordan, Oman and Kuwait – remain the epicentre of MERS-CoV’s primary infections. However, travel related incidents have been detected as well in France, Germany, Italy, Tunisia and the United Kingdom. At least, to date a total of twenty-seven countries have reported cases of MERS-CoV. To date, there has been no available vaccine or specific treatment for fighting this virus. The recommended intervention and containment strategies so far include observing basic hygiene rules, avoiding contact with infected people, regular handwashing and abstinence from camel-derived edible products.
Ebola 2014-2016
In 2014, international media attention was drawn to the outbreak of the deadly Ebola pandemic in parts of Africa. Ebola is a severe viral disease whose symptoms include fever, pain and dehydration. The virus was first detected in 1976, during two concurrent outbreaks in Sudan and the Democratic Republic of the Congo, producing 151 deaths and 280 deaths respectively. Bats are known to be the reservoir of the virus. It belongs to a family of five diverse species. Three of them – Bundibugyo (BDBV), Zaire (EBOV) and Sudan (SUDV) – are notorious for causing around twenty outbreaks in remote villages in Central Africa. The principal outbreaks took place in 1995 (254 deaths in the Democratic Republic of the Congo), 2000 (224 deaths in Uganda), 2003 (128 deaths in the Congo) and 2007 (187 deaths in the Democratic Republic of the Congo). Until the 2014 outbreak occurred, the virus had claimed 1,590 lives. The 2014 eruption, however, marked the largest outbreak of Ebola to date. It began in Guinea’s forest region, spread to neighbouring Liberia and Sierra Leone and reached their urban centers. Nigeria and Senegal experienced cases transmitted through air travel and road travel, respectively. By June 2016, when the WHO officially declared the end of the pandemic, declared cases were at least twenty-eight thousand. The number of deaths were more than eleven thousand. There is no known vaccine or treatment for Ebola, and frontline healthcare workers were the most vulnerable during the outbreak. In the recent 2014 case, the toll of the devastation was in part worsened by a confluence of governance failures: widespread poverty, poor health-care system, poor housing, inequitable resource distribution, poor housing, education and weak transport system.
Frank Afari is a doctoral student at the International History Department researching transitional Justice, human rights and reconciliation in post-colonial Ghana in the period 1957-2000, under the supervision of Professor Aidan Russell (Supervisor) and Professor Mohammad-Mahmoud Ould Mohamedou (Second Reader).
Further Reading
Alfred Jay Bollet, Plagues and Poxes – The Impact of Human History on Epidemic Disease (New York: Demos Medical Publishing, Inc., 2004)
R. Duncan-Jones, The Impact of the Antonine Plague, Journal of Roman Archaeology, 9, (1996), 108-136. (135).
Mark Harrison, Contagion: How Commerce Has Spread Disease (New Haven and London: Yale University Press, 2012).
J. N. Hays, The Burdens of Disease: Epidemics and Human Response in Western History (New Brunswick, New Jersey and London: Rutgers University Press, 2009).
J. N. Hays, Epidemics and Pandemics: Their Impacts on Human History (California: ABC-CLIO, Inc., 2005).
Edwin D. Kilbourne, “A Virologist’s Perspective on the 1918–19 Pandemic”, in H. Phillips and D. Killingray (eds), The Spanish Influenza Pandemic of 1918–19: New Perspectives (London: Routledge, 2003).
Victoria Lacroix, All About Pandemics: Epidemic of Infectious Disease (Delhi: University Publications, 2012).
Matthew L. Long, “Leprosy in Early Islam” in (eds) Darla Schumm and Michael Stoltzfus Disability in Judaism, Christianity, and Islam: Sacred Texts, Historical Traditions, and Social Analysis (New York: Palgrave Macmillan, 2011), 57.
Christian W. McMillen, Pandemics: A Very Short Introduction (New York: Oxford University Press, 2016).
J. H. Powell, Bring Out Your Dead – The Great Plague of Yellow Fever in Philadelphia in 1793 (Philadelphia: University of Pennsylvania Press, 1993).
Terence Ranger and Paul Slack, Epidemics and Ideas – Essays on the Historical Perception of Pestilence (Cambridge: Cambridge University Press, 1999).
William Rosen, Justinian’s Flea: Plague, Empire, and the Birth of Europe (New York: Viking Penguin, 2007).
Frank M. Snowden, Epidemics and Society: From the Black Death to the Present (New Haven and London: Yale University Press, 2019).
Thucydides, The Peloponnesian War (Oxford: Oxford University Press, 2009).
Nükhet Varlik, “Plague in the Islamic World, 1500–1850” in (Eds) Joseph P. Byrne, Encyclopedia of Pestilence, Pandemics, and Plagues, Volume 1 (Westport, Connecticut & London: Greenwood Press, 2008).
The Cambridge Historical Dictionary of Disease (New York: Cambridge University Press, 2003).